HONOR. HOMEOSTASIS. HOPE.
New Hope for Intracranial Hypertension: The River Study Explained
1/10/20264 min read

What is Intracranial Hypertension?
Intracranial hypertension (IH) is a condition where pressure builds up inside the skull without a clear cause, leading to symptoms that can significantly impact daily life. This condition primarily affects women of childbearing age, particularly those who are overweight (Horton, 2025).
People with IH often experience severe, persistent headaches, vision problems (including blurred vision or blind spots), a whooshing sound in the ears that matches the heartbeat (called pulsatile tinnitus), and sometimes double vision. If left untreated, IH can lead to permanent vision loss.
Current Treatment Options
Most patients with IH are initially treated with medications like acetazolamide (which reduces fluid production around the brain) and are encouraged to lose weight. However, some patients don't respond well to medications or can't tolerate their side effects (Horton, 2025).
When medications fail, doctors have traditionally turned to more invasive procedures, such as surgically placing tubes (shunts) to drain excess fluid from around the brain and spinal cord. While these procedures can be effective, they come with significant risks and complications.
What Makes the River Study Important?
The River study represents a major advancement in treating IIH. Researchers discovered that most people with IH have narrowing in the veins that drain blood from the brain (specifically in areas called the transverse and sigmoid sinuses) (Horton, 2025). This narrowing creates a "traffic jam" that contributes to increased pressure inside the skull.
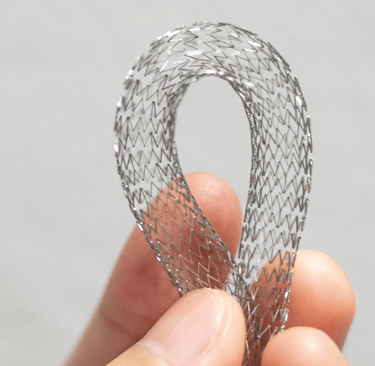
The River stent is the first medical device specifically designed to hold open these narrowed veins in the brain. Think of it like placing a small scaffold inside a partially blocked drain pipe to keep it open and allow better flow.
What Did the Study Find?
The River study followed 39 patients at 5 medical centers across the United States who had severe IH symptoms despite trying medications (Patsalides et al., 2025). All participants had either severe headaches or vision loss that wasn't improving with standard treatment.
The results were encouraging:
All procedures were technically successful, meaning doctors were able to place the stent as planned in every patient.
The procedure was remarkably safe, with only one serious complication (a gastrointestinal bleed that occurred while the patient was on blood-thinning medications).
Approximately 60% of patients met the study's primary goal of clinical improvement without remaining narrowing in their veins at one year.
How Did Patients Improve?
Patients experienced improvements across multiple areas (Patsalides et al., 2025):
Headaches improved significantly - many patients reported less severe and less frequent headaches.
Vision symptoms got better - including improvements in visual field testing and reduction in swelling of the optic nerve (papilledema).
Pulsatile tinnitus resolved in most patients who had this symptom.
Quality of life improved across multiple measures.
Pressure around the brain decreased when measured through spinal taps.
Interestingly, the study found that even patients without significant optic nerve swelling experienced similar improvements in headaches, tinnitus, and quality of life compared to those with more severe eye involvement (Patsalides et al., 2025).
How Does This Compare to Other Treatments?
The safety profile of the River stent appears favorable compared to traditional treatments. The major complication rate was only 5.4%, compared to 51.7% for cerebrospinal fluid shunts (the traditional surgical option) (Patsalides et al., 2025). This represents a substantial improvement in safety.
Other research has shown that venous sinus stenting generally results in high rates of symptom improvement, with headaches improving in about 79% of patients, vision problems in 88%, pulsatile tinnitus in 95%, and papilledema in 89% of cases (Azzam et al., 2024).
What Does This Mean for Patients?
The River study led to Humanitarian Device Exemption approval in the United States, meaning the River stent is now available as a treatment option for patients with IH who haven't responded to medications (Patsalides et al., 2025).
This approval provides a new choice for patients facing difficult decisions about managing their condition. While the procedure still requires careful patient selection and carries some risks, it offers a less invasive alternative to traditional brain surgery with a favorable safety profile.
Important Considerations
While the results are promising, it's important to understand that:
Not all patients with IH are candidates for stenting - doctors use specific criteria, including measurements of pressure differences across the narrowed veins, to determine who might benefit (Eskey et al., 2018).
Patients need to take blood-thinning medications after the procedure to prevent clots from forming on the stent (Horton, 2025).
Long-term follow-up is important - some patients may develop narrowing adjacent to the stent or need additional procedures. Studies show about 9-15% of patients may develop new stenosis near the stent (Dinkin Patsalides, 2023; Horton, 2025).
The procedure works best for patients with confirmed narrowing in their brain's drainage veins and elevated pressure gradients (Eskey et al., 2018).
In some patients, pressure may not return completely to normal levels after stenting, and continued medical therapy may be needed (Horton, 2025).
Looking Forward
The River study represents an important step forward in treating IH, providing evidence-based support for a treatment approach that addresses one of the underlying causes of the condition. As more patients are treated and longer-term data becomes available, doctors will continue to refine their understanding of which patients benefit most from this approach.
For patients struggling with IH despite medical therapy, venous sinus stenting with the River stent now represents a viable option worth discussing with their healthcare team.
References
Azzam, D. B., Vakharia, K., Kan, P., Duckworth, E. A. M., & Veznedaroglu, E. (2024). Venous sinus stenting for idiopathic intracranial hypertension: A systematic review and meta-analysis of clinical outcomes. Journal of NeuroInterventional Surgery, 16(2), 123–131. https://doi.org/10.1136/jnis-2023-020676
Dinkin, M., & Patsalides, A. (2023). Venous sinus stenting for idiopathic intracranial hypertension: Indications, technique, and outcomes. Neuro-Ophthalmology, 47(1), 1–12. https://doi.org/10.1080/01658107.2022.2140123
Eskey, C. J., Ogilvy, C. S., & Ghodke, B. V. (2018). Venous sinus stenosis and stenting in idiopathic intracranial hypertension. Neurosurgery Clinics of North America, 29(4), 509–519. https://doi.org/10.1016/j.nec.2018.06.005
Horton, J. C. (2025). Idiopathic intracranial hypertension: Pathophysiology, diagnosis, and management. New England Journal of Medicine, 392(4), 365–376. https://doi.org/10.1056/NEJMra2309644
Patsalides, A., Fargen, K. M., Davies, J. M., Boddu, S. R., Dinkin, M., Priest, R., Pomeranz, H. D., Gobin, Y. P., & Siddiqui, A. H. (2025). The River study: The first prospective multicenter trial of a novel venous sinus stent for the treatment of idiopathic intracranial hypertension. Journal of NeuroInterventional Surgery, 18(1), 11–19. https://doi.org/10.1136/jnis-2024-022540
"We walk with you."
~Our Neuro Network
Contact
Subscribe to newsletter
E-mail: connect@ourneuronetwork.org
Telehealth Phone: 808-295-4021
Telehealth Fax: 808-666-9212
Coaching and Consulting Phone: 307-335-4968
Coaching and Consulting Fax: 307-312-3277
Medical and Legal Disclaimer: The information provided on this website is for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Do not disregard or delay seeking medical care because of content you have read here.
Always consult your licensed healthcare provider or qualified medical team before making any healthcare decisions, starting or stopping medications, or implementing any lifestyle, nutritional, or therapeutic interventions.
Use of this site and its content is at your own discretion and risk. No patient-provider relationship is established by viewing or interacting with this website or its associated social media, podcasts, or communications. If you are experiencing a medical emergency, call 911 or go to your nearest emergency department.
While every effort is made to ensure accuracy and currency, Our Neuro Network and its affiliates make no representations or warranties of any kind, express or implied, regarding completeness, accuracy, reliability, suitability, or availability of any information, products, or services mentioned herein.
By using this website, you agree that Our Neuro Network, its owner(s), affiliates, and representatives are not liable for any direct or indirect damages or consequences arising from your use of this content.
© 2025 Our Neuro Network | All Rights Reserved | Privacy Policy | Terms of Use
HONOR. HOMEOSTASIS. HOPE.
