HONOR. HOMEOSTASIS. HOPE.
A Holiday Message From a Place of Truth, Care, and Hope
Content Note: This post discusses chronic neurologic illness, depression, suicide risk, and loss. Support resources are included.
12/20/20256 min read

Content Note
This post discusses chronic neurologic illness, depression, suicide risk, and loss. Support resources are included.
A Holiday Message From a Place of Truth, Care, and Hope
I wish all of my family, friends, and community a very peaceful holiday season. I would love to travel to Arkansas and Tennessee to celebrate and enjoy my family's company, but my medical condition and current treatment require that I remain home for now, prioritizing balance, health, and recovery.
The truth is, I did not do anything particularly special on Thanksgiving, and I plan to lay low on Christmas as well. Intracranial hypotension profoundly depletes energy, and forcing activity can worsen symptoms and increase the risk of ongoing or recurrent cerebrospinal fluid (CSF) leak.
Why the Holidays Can Be Especially Hard With Neurologic Illness
The holidays are often especially challenging for patients living with spontaneous intracranial hypotension (SIH), spinal CSF leak, idiopathic intracranial hypertension (IIH), cerebral venous congestion, and inherited neurometabolic syndromes. These conditions directly affect the brain.
Intracranial hypotension can contribute to depression due to the literal sagging of the limbic system and brainstem within the skull base. These structures regulate homeostasis, mood, autonomic function, and survival responses. When placed under sustained physiologic stress, their function can become dysregulated, resulting in measurable neuropsychiatric symptoms (Volz et al., 2024).
Studies of SIH and spinal CSF leak consistently demonstrate severe symptom burden, reduced quality of life, depression, anxiety, and reported suicidality, with improvement following effective treatment of the underlying CSF leak (Liaw et al., 2023; Volz et al., 2024). Many patients look and feel depressed because of disease physiology, not because of weakness, lack of gratitude, or inability to cope.
Acknowledging this reality allows for better care and far less shame.
How I Actively Support My Mental Health
Because of the known neurologic and psychiatric risks associated with my condition, I am intentional about mental health protection. My personal toolkit includes:
Consistent nutrition and hydration, emphasizing regular meals rich in vitamins and essential nutrients, and intentionally avoiding skipped meals to support neurologic stability and energy balance.
A regular sleep schedule, with intentional and consistent bedtimes and wake times to support circadian rhythm, neurologic recovery, and overall homeostasis.
Prayer and/or meditation, practiced regularly to support grounding, meaning, and emotional regulation.
Journaling, as a tool for reflection, emotional processing, and cognitive clarity during periods of stress or instability.
Vagal nerve stimulation and nervous-system regulation exercises, used intentionally to support limbic system balance, autonomic regulation, and resilience during physiologic stress.
Ongoing care with a therapist or counselor, with regularly scheduled visits and additional sessions as needed during periods of increased vulnerability.
Connection with loved ones through accessible means, such as phone calls, video visits, and social media, recognizing that connection does not require physical presence to be meaningful or protective.
Avoidance of major decisions during periods of medical or emotional instability, with intentional delay when possible and consultation with trusted supports when decisions cannot wait.
Reliance on trusted sources of support, including family, close friends, and mental health professionals, when clarity, grounding, or perspective is needed.
Open acknowledgment of depression or emotional struggle related to illness, recognizing that while the condition is not my fault, naming the truth and seeking support is within my power and protective of my well-being.
Complete avoidance of alcohol, recognizing its negative effects on neurologic stability, mood regulation, and judgment.
Avoidance of street drugs, due to lack of quality control, unpredictable effects, and increased risk of harm in the setting of neurologic disease.
Use of lifestyle-based interventions and prescribed treatments, including nervous-system regulation strategies and medications, overseen and approved by my healthcare team.
A written emergency action plan, to be activated if suicidal thoughts arise, including contacting trusted supports, notifying my therapist, and accessing the 988 Suicide & Crisis Lifeline.
Having an action plan does not mean it will be needed. It means risk is acknowledged honestly and safety is prioritized with intention and compassion.
Suicide Risk in Neurologic and Neurometabolic Disease
Patients with idiopathic intracranial hypertension face a significantly increased risk of death by suicide compared with the general population, as demonstrated in registry-based mortality studies (Hermes et al., 2020). This finding confirms that suicide risk in IIH is measurable, clinically significant, and demands proactive attention.
In spontaneous intracranial hypotension and spinal CSF leak, formal suicide mortality rates are less well quantified. However, peer-reviewed studies consistently document severe mental health burden, including depression, anxiety, disability, and reported suicidality, with improvement following effective treatment of the underlying CSF leak (Liaw et al., 2023; Volz et al., 2024). These findings support the need for routine mental health screening, safety planning, and timely medical treatment in this population.
Inherited neurometabolic syndromes are associated with clinically meaningful neuropsychiatric manifestations, including depression, anxiety, and cognitive dysfunction, due to direct effects of metabolic dysregulation on the brain (Pan et al., 2013; van de Burgt et al., 2023). While suicide rates are not uniformly quantified across these rare conditions, the psychiatric burden alone warrants vigilance, education, and prevention-focused care.
Thoughts of suicide can affect anyone, particularly when neurologic disease alters brain chemistry, physiology, and decision-making capacity. Open discussion of this risk does not increase suicide. Silence does.
Many individuals who die by suicide do so during periods of acute physiologic or psychological crisis, when judgment is impaired. This reality underscores the importance of emergency action plans, delaying irreversible decisions during instability, and prioritizing treatment of the underlying medical condition.
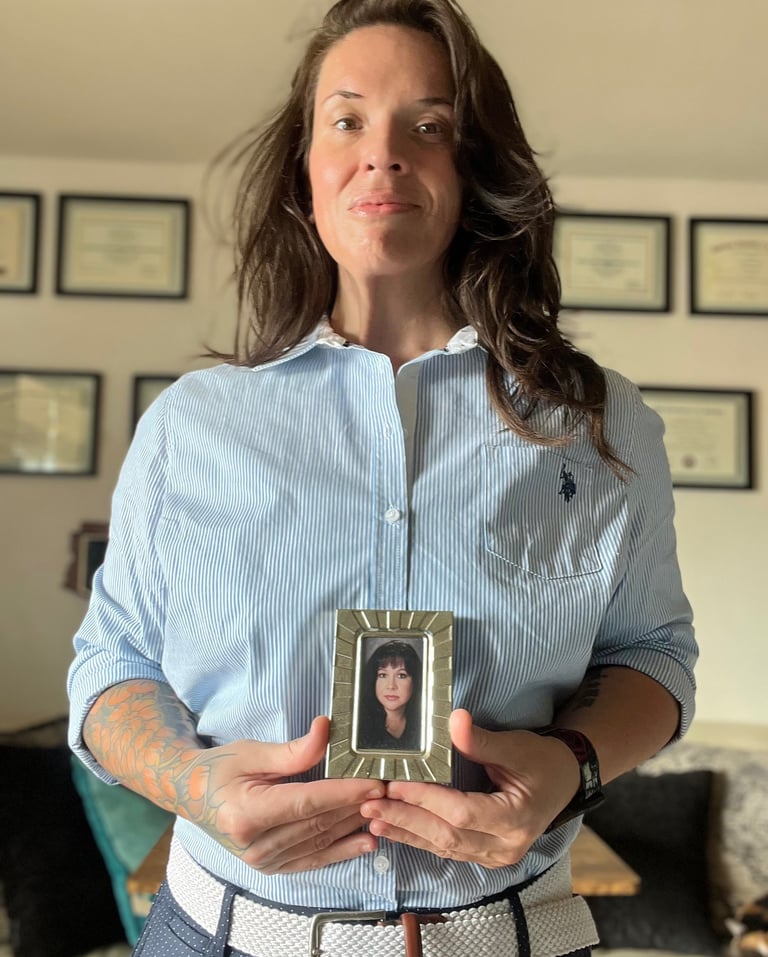
I believe my mother’s suicide was driven by disease-related limbic instability. If she had been at her baseline—her healthiest and most regulated self—she would not have chosen that path. Suicide harms not only the individual, but generations of loved ones, and it increases risk within families.
Acknowledging this truth has helped me manage depression and suicidality that can naturally accompany my disease. It creates accountability to protect myself and builds a system of support rather than isolation.
On Dignity, Palliative Care, and Ethical Compassion
I have pledged to myself and my loved ones that I will not take my life as long as I am consciously able to make that decision. I have also openly discussed the role of palliative care and hospice for individuals who are nearing the end of life or have no hope for meaningful recovery.
Choosing comfort-focused care in those circumstances is not suicide. It is allowing natural death with dignity.
Most people who wish they would not wake up feel that way because physical or psychological suffering feels overwhelming and unending. Many neurologic and neurometabolic conditions are treatable, though navigating care takes time, advocacy, and support.
Quality-of-life programs must exist alongside mental health services. Most patients experiencing suicidality need improved treatment of their underlying condition to restore homeostasis. For those who truly reach the end of meaningful recovery, compassionate palliative and hospice care must be accessible so no one feels driven toward traumatic or violent ends.
Holding Truth and Hope Together
The holidays can be especially difficult when illness enforces isolation. Naming this truth allows space for compassion and resilience.
I look forward to visiting my family after recovery from my next surgery, when I can fully enjoy time together. That visit will be a celebration. Recovery permitting, I also plan to formally launch Our Neuro Network in April.
Truth and hope can coexist. Our greatest challenges often carry within them the fuel for transformation.
My disease, its impact on my family, and my mother’s suicide do not define or limit me. They compel me to prioritize truth, comfort, dignity, and life, especially during times of instability.
Support Resources
If you are struggling or feeling unsafe, help is available.
In the United States, call or text 988 to reach the Suicide & Crisis Lifeline.
If you are outside the United States, local crisis services can provide support.
From the Our Neuro Network perspective, advocacy means telling the truth, reducing stigma, protecting life, and promoting ethical, compassionate care across the continuum.
References (APA 7th)
Hermes, S. M., et al. (2020). Mortality among patients with idiopathic intracranial hypertension enrolled in the Intracranial Hypertension Registry. Neurology, 95(20), e2743–e2754.
https://doi.org/10.1212/WNL.0000000000010858
Liaw, V., et al. (2023). Quality of life in patients with confirmed and suspected spontaneous intracranial hypotension and spinal cerebrospinal fluid leak. Journal of Neurosurgery, 139(2), 1–10.
https://thejns.org/view/journals/j-neurosurg/139/2/article-p1.xml
Pan, L., et al. (2013). Neuropsychiatric symptoms in inborn errors of metabolism. Molecular Genetics and Metabolism, 110(1–2), 1–7.
https://doi.org/10.1016/j.ymgme.2013.07.004
van de Burgt, N., et al. (2023). Psychiatric manifestations of inborn errors of metabolism. The Lancet Psychiatry, 10(6), 447–458.
https://doi.org/10.1016/S2215-0366(23)00102-8
Volz, F., et al. (2024). More than a headache: Somatic and mental symptom burden in spontaneous intracranial hypotension and improvement after leak closure. Frontiers in Neurology, 15, 1421579.
https://doi.org/10.3389/fneur.2024.1421579
"We walk with you."
~Our Neuro Network
Contact
Subscribe to newsletter
E-mail: connect@ourneuronetwork.org
Telehealth Phone: 808-295-4021
Telehealth Fax: 808-666-9212
Coaching and Consulting Phone: 307-335-4968
Coaching and Consulting Fax: 307-312-3277
Medical and Legal Disclaimer: The information provided on this website is for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Do not disregard or delay seeking medical care because of content you have read here.
Always consult your licensed healthcare provider or qualified medical team before making any healthcare decisions, starting or stopping medications, or implementing any lifestyle, nutritional, or therapeutic interventions.
Use of this site and its content is at your own discretion and risk. No patient-provider relationship is established by viewing or interacting with this website or its associated social media, podcasts, or communications. If you are experiencing a medical emergency, call 911 or go to your nearest emergency department.
While every effort is made to ensure accuracy and currency, Our Neuro Network and its affiliates make no representations or warranties of any kind, express or implied, regarding completeness, accuracy, reliability, suitability, or availability of any information, products, or services mentioned herein.
By using this website, you agree that Our Neuro Network, its owner(s), affiliates, and representatives are not liable for any direct or indirect damages or consequences arising from your use of this content.
© 2025 Our Neuro Network | All Rights Reserved | Privacy Policy | Terms of Use
HONOR. HOMEOSTASIS. HOPE.
